Overview
Displacement puts significant psychological and social stress on individuals, families and communities. People may have experienced multiple atrocities and adversities prior to or during flight. Once they reach safety, their current living conditions may also impose significant stress and hardship, often coupled with worries about those left behind and concerns about the future. This leads to increased levels of mental health conditions and psychosocial problems.
The term ‘mental health and psychosocial support' (MHPSS) refers to any type of local or outside support that aims to protect or promote psychosocial well-being or prevent or treat mental health conditions. MHPSS is not confined to a single sector but requires a multi-sectoral approach with involvement of partners in health, education and protection (community-based protection, child protection and GBV). Addressing MHPSS issues requires that:
- emergency responses are safe, dignified, participatory, community owned, and socially and culturally acceptable.
- people are enabled to attend to their own well-being and that of others in their families and communities.
- persons distressed by mental health and psychosocial problems have access to appropriate support and care.
- persons suffering from moderate or severe mental health conditions have access to essential mental health services and to social care.
Relevance for emergency operations
People affected by humanitarian emergencies often face pervasive psychological stress that causes widespread emotional suffering and may undermine people’s ability for survival. The loss and stress experienced during humanitarian emergencies cause grief, fear, anxiety, guilt, shame and hopelessness that overtax individuals' capacity to cope. Community structures that regulate community well-being, such as extended family systems and informal community networks, may break down. This can cause or exacerbate social and psychological problems. Significant stress over long periods, harms the development of children, increases the risk that they will have physical or mental health problems, and may contribute to educational difficulties later in life.
Humanitarian emergencies increase the risk of developing mental health conditions, including depression, posttraumatic stress disorder, and alcohol and substance use conditions, all of which weaken the ability of individuals to fend for themselves and care for others who depend on them. During emergencies, people with severe mental disorders (psychosis, bipolar disorder, severe forms of depression or posttraumatic stress), or intellectual and developmental disabilities, have elevated protection risks if they experience neglect, abandonment, homelessness, sexual or domestic abuse, social stigma, or are excluded from humanitarian assistance, education, livelihood opportunities, healthcare or other services. Those who care for people with severe mental health conditions can experience extreme distress, isolation and strain on financial and other resources.
MHPSS is not an optional ‘nice to have’ intervention but an essential part of the emergency response. How that response is shaped is strongly influenced by operational factors such as: available resources, presence of partners with experience in MHPSS and capacity of the national systems.
Main guidance
a) Emergency Phase
MHPSS as a multi-layered system
MHPSS is not a separate sector, but an integrated part of programmes in various sectors. This is visualized in the MHPSS pyramid (Illustration 1), which shows several layers of complementary support, with referral systems between the layers. It is important to pay attention to all layers, ranging from interventions that benefit all people to targeted interventions for specific groups.
Illustration 1: Pyramid of multi-layered mental health and psychosocial support
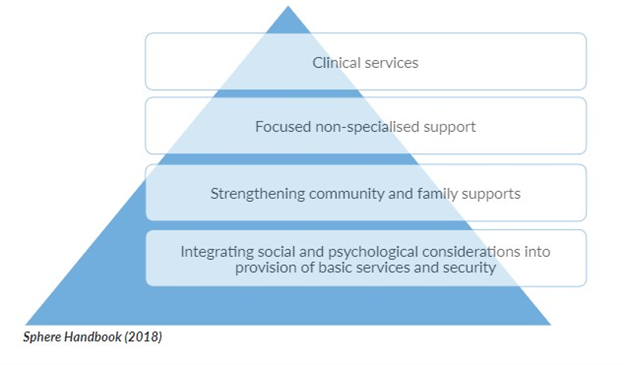
Layer 1: Provision of basic services and security in ways that protects the dignity of all people, including those who are particularly marginalized or isolated and who may face barriers to accessing services and deliver the response in a participatory, rights-based way using Age, Gender and Diversity (AGD) approaches.
Layer 2: Strengthening community and family support: enabling people to preserve and promote their psychosocial well-being through activities that foster social cohesion and through enabling communities to restore or develop mechanisms to protect and support themselves.
Layer 3: Provision of focused psychosocial support through individual, family or group interventions to those who find it difficult to cope within their own support network. Non-specialised workers usually deliver such support, after training and with ongoing supervision.
Layer 4: Clinical mental health and psychosocial services for those with severe symptoms or whose intolerable suffering rendering them unable to carry out basic daily functions. Such interventions are usually led by mental health professionals but can also be done by trained and supervised general health workers.
- Adopting an MHPSS approach implies providing humanitarian assistance in ways that support the mental health and psychosocial well-being of persons of concern. MHPSS is relevant for all humanitarian actors and all forms of humanitarian action.
- Integrating MHPSS interventions. This implies focusing on activities with the primary goal of improving the mental health and psychosocial well-being of persons of concern. Such activities are usually implemented in health, community-based protection, GBV, child protection, and education.
Key steps
It is important to build understanding of MHPSS in UNHCR and among partners in all sectors, to reduce the burden of mental illness, improve the ability of displaced populations to function and cope, and strengthen resilience. To this end, it is important to adopt an ‘MHPSS approach’ and integrate ‘MHPSS interventions’ in field operations as a priority. This section describes the key steps to be taken.
i. Include MHPSS elements in assessments
Initial rapid assessments for health and protection should include MHPSS elements, to increase understanding of the MHPSS problems refugees face, their ability to deal with them, the resources that are available, and the kind of responses required.
Tips for doing MHPSS assessments:
- Make assessments participatory; involve persons of concern at every stage, with a particular focus on including more isolated or marginalized individuals.
- Assess both MHPSS needs and MHPSS resources. Focus on problems but also on coping mechanisms and formal and informal sources of support.
- Apply a broad definition of MHPSS. Assessments that narrowly focus only on one mental disorder, such as post-traumatic stress disorder (PTSD), do not provide the data needed to design a comprehensive MHPSS programme.
- Do not try to estimate the prevalence of mental disorders during an emergency because such an assessment is methodologically complicated, requires specific resources and, most important, is not essential to start implementing services.
- When integrating MHPSS questions in quantitative surveys such as Multi-Sectoral Needs Assessments, consider using:
- The six questions of the WHO-UNHCR Assessment Schedule of Severe Symptoms in Humanitarian Settings (WASSS) (tool 2 in Assessing Mental Health and Psychosocial Needs and Resources: Toolkit for Humanitarian Settings (WHO & UNHCR 2012 Page 38-39).
- A single MHPSS Question (as was used in Multisector Needs Assessments in the Ukraine Regional Refugee Response) MHPSS Question for Multisector Needs Assessment
- As a rule of thumb, use WHO projections of mental disorders in adult populations affected by emergencies (Box 1)
Box 1: Point prevalence estimates for mental disorders in conflict-affected populations, adjusted for comorbidity
| Point prevalence | |
|---|---|
| Severe disorder (severe anxiety, severe post-traumatic stress disorder, severe depression, schizophrenia, and bipolar disorder) | 5·1% |
| Moderate disorder (moderate anxiety, moderate post-traumatic stress disorder, and moderate depression) | 4·0% |
| Mild disorder (mild anxiety, mild post-traumatic stress disorder, and mild depression) | 13·0% |
| Total | 22·1% |
| Source: Charlson et al 2019, New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet, 394: 240-248 | |
ii. Promote the adoption of an MHPSS approach throughout the work of UNHCR and partners
- Employing a participatory approach and providing services respectfully can improve the psychosocial well-being of persons of concern; but staff involved in a refugee response may not always be aware of these effects. It is important to ensure that all stakeholders in UNHCR-supported programmes are aware that MHPSS is a cross-cutting issue.
- Improving staff awareness of and information on MHPSS, including the awareness of staff in reception centres and registration desks, can be achieved by seminars or training. Relevant themes include: effective communication, dealing with strong emotions, and identifying MHPSS problems in persons of concern.
- Build inter-sectoral capacity to integrate MHPSS. For example:
- Provide half or one day orientation seminars on psychological first aid (PFA) using the facilitator guide. Tools
- Psychological First Aid. Guide for field workers
- Psychological first aid: facilitator’s manual for orienting field workers
- Integrate MHPSS in the regular training programmes for staff working on gender-based violence (GBV), Child Protection and Community-Based Protection
- Provide half or one day orientation seminars on psychological first aid (PFA) using the facilitator guide. Tools
- Inform managers about the importance of using MHPSS approaches in all sectors. Consider holding short briefing sessions for senior management.
- Ensure that groups or individuals with specific MHPSS needs can access basic services (including food and non-food distributions). If necessary and appropriate, arrange separate queuing systems or a ‘buddy/helper' system; monitor the distribution of goods to groups or individuals with specific needs to ensure that distribution is safe, dignified and equitable.
iii. Design and implement MHPSS interventions within health programmes
The provision of services for mental health and psychosocial support is a regular and integral part of primary health care services. (See: UNHCR Administrative Instruction on Public Health Programming and UNHCR Global Public Health Strategy 2021-2025). In general, this implies that, as much as possible, one partner provides a comprehensive package of primary health care that includes essential mental health services. Specialized MHPSS partners may be required in contexts with complex mental health needs that cannot be met through the national system.
For general health programmes
- Ensure that mental health is included in Project Partnership Agreements with health providers
- Arrange supply of essential medication for mental disorders to health facilities, at a minimum one anti-epileptic, one antipsychotic (plus anticholinergic), one antidepressant and one anxiolytic medication.
- Organize training for general health staff in identifying and managing priority mental health conditions. Such trainings usually take 3-5 days and need to be followed by supportive supervision and refresher trainings. Tools:
- WHO/UNHCR (2015) mhGAP Humanitarian Intervention Guide (available in various languages)
- WHO/UNHCR (2022) Facilitation Manual mhGAP Humanitarian Intervention Guide (available also in French)
- Arrange for a mental health professional (psychiatrist, psychiatric clinical officer, psychiatric nurse) to support the primary health care facilities to manage people with complex conditions and provide clinical supervision to general health workers. As a rule of thumb, a mental health professional should be made available in refugee camps or settlements with more than 25,000 inhabitants. This professional can be an NGO staff or an employee of a governmental mental health service.
- Ensure that consultations for mental health conditions are registered in the health information system. If UNHCR’s integrated refugee health information system (iRHIS) is used, make sure that the mental health categories are used. In case mental health consultations are done by a separate MHPSS partner, their data should be included in the iRHIS or other health information systems.
- Enable community health workers (CHW) to provide basic MHPSS interventions. Mental health needs to be a part of the training curriculum and they should be regularly supervised on mental health issues. They can be trained to:
- provide Psychological First Aid and Basic Psychosocial Skills to people in acute distress. Suggested tools see above under b)
- Identify and refer people with severe and complex mental health issues that threaten survival.
In some operations, specialized community MHPSS volunteers are trained to do focused work.
For partners with dedicated MHPSS expertise:
Where partners are available with dedicated MHPSS expertise:
- Take steps to make brief psychological therapies available to people impaired by prolonged distress: consider starting with evidence-based brief psychological therapies for mild and moderate mental health conditions. (See box 2)
- Arrange a referral pathway to these service from the general health providers to the MHPSS partner.
- Ask MHPSS partner to build MHPSS capacity in general partners for health and protection.
For more information, see the Entry on health responses.
Box 2: Psychological interventions Brief scalable psychological interventions (5-8 sessions) can be delivered by non-specialized staff after a brief training and with supportive clinical supervision by a mental health professional. There are several scalable psychological methods. SEE ANNEX B of Global Public Health Strategy. One of the most widely used methods is Problem Management Plus (PM+) which is based on Cognitive Behavioral Therapy, which teaches the participants four techniques to cope better with symptoms of depression and anxiety:
PM+ is provided in five sessions of 90 min and can be delivered in individual format or group format. It has been translated in many languages. |
iv. Include MHPSS interventions in community-based protection
Most communities already employ protection measures to support members facing heightened protection risks. Emergency displacement can undermine such community-based support interventions. Engaging together in response activities can help community members to restore feelings of agency and hopefulness, strengthen social connections and provide a sense of collective identity and belonging, factors that promote well-being and recovery. At the same time, certain coping strategies may harm or disadvantage marginalized groups (for example measures that restrict women's rights or exclude minority groups).
- Discuss MHPSS strengths, needs, and challenges with the community, using culturally and contextually relevant terminology and concepts and accessible communication formats and channels.
- Support (re)establishment of community initiatives that promote mental health and psychosocial well-being (e.g. cultural and religious activities, self-help initiatives and support groups, appropriate communal healing practices, communal arts-based activities, etc.) and partner with these initiatives to strengthen their capacity to respond to MHPSS needs (e.g. providing safe spaces in which to convene, capacity-building in MHPSS and/or group facilitation skills, using an Age Gender and Diversity - AGD - approach).
- Integrate MHPSS in other community interventions such as sport activities, vocational training and literacy classes that can support development of coping mechanisms to alleviate stress and introduce psychosocial support projects in multi-purpose community centres.
- Recruit and train staff and volunteers from community groups to reach and support individuals with mental and psychosocial concerns from all AGD groups.
- Promote and support activities that reduce tensions within communities of displaced persons (I.e. tensions between ethnic groups in a refugee or IDP camp), and between displaced persons and host community members.
- Take steps to integrate people with severe mental health conditions, persons with psychosocial, intellectual and developmental disabilities and epilepsy in programmes for community-based rehabilitation; provide support to enable them to participate in mainstream programmes. Work with communities to reduce discrimination against people with mental health conditions and address social norms that stigmatize mental health or psychosocial support needs.
For more information, see the Entry on community-based protection.
v. Design and implement MHPSS interventions within child protection programmes
It is important to ensure that children at risk, and separated and unaccompanied children, are identified and referred to relevant services, including best interest procedures and multi-sectoral services. Such children should receive appropriate psychosocial support, including individual, family and group-based interventions appropriate to their needs, and where necessary refer family members to appropriate psychosocial or mental health services. Six core actions underpin UNHCR’s field-focused programming around child protection and MHPSS in emergencies:
- Coordinate MHPSS within & across sectors. See section viii below. This includes creating joint referral pathways to facilitate access of children and care takers to MHPSS services and activities and to additional support as needed. It also includes facilitating a dialogue between government and humanitarian actors to establish MHPSS-specific roles and responsibilities in the emergency response.
- Disseminate key messages to promote MHPSS & well-being for children, families and communities. This includes providing information for parents and caregivers about MHPSS distress and how they can support their children.
- Orient frontline child protection workers & community actors in basic psychosocial support skills. This includes familiarizing frontline workers and community leaders with local referral pathways and available mental health and psychosocial support services for children and caregivers.
- Provide MHPSS through case management services. This includes educating the child and their caregivers about mental health, coping strategies, and available support services. It also includes engaging and involving the child's caregivers and significant family members in MHPSS case management and ensuring a smooth transition and continuity of care when the child moves between different services or stages of the case management process.
- Support new & pre-existing group-based community MHPSS activities. This includes establishing structured recreational activities, led by community volunteers, and coordinate these with education activities.
- Promote caregivers´ mental health and psychosocial well-being and strengthen their capacity to support children. This includes providing parents and caregivers with information on children's and their own emotions and behaviour in emergencies and explain how they can help their children and themselves to recover, and access services. Additionally, it is advised where possible to support community-based early childhood care and development programmes, to ensure that mothers of very young children are enabled to provide appropriate protection, care, stimulation and support. Where relevant, link these activities to nutrition and breast-feeding programmes.
For more information, see the Entry on Child protection and link to the forthcoming ‘Guidance Note on Child protection and MHPSS’.
vi. Design and implement MHPSS interventions within programmes for GBV prevention and response
- Establish (group) psychosocial activities within Women and Girls’ Safe Spaces (WGSS) with a focus on women and girls’ empowerment. These activities can also serve as non-stigmatizing entry points to case management for GBV survivors.
- Boys’ survivors can access support through Child Friendly Spaces or other relevant MHPSS partner trained on Caring for Child Survivors. Adult male survivors can receive assistance at designated community centres where MHPSS services are available, in health centres, or other non-stigmatizing entry points where qualified personnel is available.
- Ensure that survivors have safe access to individual or group psychosocial services including those that promote resilience strategies (e.g. women support groups/networks).
- Ensure that quality and survivor centred MHPSS services are included in the GBV referral pathway. Training GBV workforce (and medical staff involved in clinical management of rape survivors) to recognize and respond to signs of emotional distress of women/girls (psychological first aid) and to recognize signs indicating that women/girls may benefit from GBV case management or specialized mental health care.
- If survivors wish, facilitate referral to trained providers of evidence-based psychotherapies for survivors who are not functioning well because of their symptoms of mental health conditions such as depression and stress-related conditions.
- If survivors wish, provide clinical care with follow-up for survivors who have developed moderate to severe mental health conditions (by mental health-care providers with appropriate training in the provision of mental healthcare to survivors of GBV).
- Ensure GBV risks are effectively mitigated across all MHPSS programming in line with the IASC Guidelines for Integrating GBV Interventions in Humanitarian Action.
For more information, see the Entry on GBV Mitigation and Response.
vii. Design and implement MHPSS interventions (including Social and Emotional Learning – SEL) within education programmes
Providing educational activities to children and youth from the early stages of an emergency can reduce psychosocial and mental health impacts of extreme stressors and displacement by restoring routine and normalcy and creating hope for a better future. Fostering the development of social and emotional skills and competences and supporting the provision of school-based mental health and psychosocial services (MHPSS) are essential to child development and well-being, which require attention from the start of an emergency.
- Create conditions in learning spaces that foster social and emotional learning (SEL) allowing learners to improve mood, concentration, ability to learn and develop healthy relationships. These can be created through both teacher-led and learner-led interventions.
- Promote an environment where learners in need have access to mental health services and psychosocial support. This requires the development of functional referral pathways and close coordination of education, child protection actors and child-focused MHPSS services.
- Where feasible, integrate psychosocial/ recreational activities into programmes delivered through temporary learning spaces and organize social and cultural events, including sports activities, in schools and non-formal education programmes, to foster social connectedness among children, parents, and the community.
- Promote the establishment and operation of learning environments that learners perceive as accessible, safe and conducive. Consider both physical infrastructure (well-built, disability-friendly classrooms and separate latrines for boys and girls) and the school's culture. Take measures to stop discrimination against vulnerable learners and learners with psychosocial or other disabilities.
For more information, see the Entry on education in emergencies URBAN and CAMPS and the following resources:
- Education 2030: A Strategy for Refugee Education (UNHCR, 2019)
- MHPSS and Education in Emergencies Toolkit (MHPSS.net, 2021)
viii. Establish coordination mechanisms for MHPSS
In emergencies it is important to establish or maintain a multi-sectoral MHPSS coordination mechanism, adequate to the context and number of agencies implementing MHPSS. Especially in larger emergencies where there are multiple MHPSS actors, this could be a single cross-sectoral MHPSS Technical Working Group (MHPSS TWG) which should be established early in the emergency response. This group may be co-led by a health and a protection humanitarian organization and/or a governmental organization when feasible. If a major refugee emergency does not have an MHPSS TWG, UNHCR should consider creating one. The MHPSS Technical Working Group (TWG) should promote the coordination of MHPSS activities across both national actors (e.g., CBOs, government) and international actors (e.g., INGOs, UN agencies), provide technical input, and help to ensure consistent standards and quality within MHPSS work. It is not recommended to establish separate MHPSS coordination mechanism focusing only on one sector (such as health or child protection). In large or complex emergencies, consider requesting an interagency deployee to support coordination and capacity building (See box 3).
For more information, especially in mixed coordination, see:
Box 3: MHPSS Surge Support MHPSS Dutch Surge Support (DSS) is a programme that deploys Mental Health and Psychosocial Support (MHPSS) experts to assist in relief efforts for a few weeks up to several months during or after a humanitarian crisis. DSS MHPSS work to strengthen interagency cooperation on multisectoral mental health and psychosocial support in armed conflict, refugee crises, and natural disasters. Experts can be hosted by various agencies including UNHCR, but will not work exclusively for that organization. Deployment request are done through HR units through the UNHCR Division of Emergency Support and Supplies in consultation with the Snr MHPSS Officer, See more here. |
Post emergency phase
In the post emergency phased the emphasis shifts to sustainable treatment coverage across the affected areas through, inter alia, strengthening existing national mental health systems and fostering inclusion of marginalised groups (including refugees) in these systems (ref. Sphere Handbook - Mental Health Standard 2.5 Mental health care). See the Annex B (MHPSS) in the Global Public Health Strategy.
Checklist: MHPSS Coordination
Set up a system for multi sectoral MHPSS coordination.
If a Technical Working Group (TWG) for MHPSS is established in a refugee emergency, consider UNHCR to co-chair.
Ensure that a representative of the MHPSS TWG provides updates to coordination meetings for protection (including child protection) and health.
Standards
Sphere Mental health standard (2018)
People of all ages have access to healthcare that addresses mental health conditions and associated impaired functioning.
In the Sphere Handbook, MHPSS is mentioned throughout the document, in addition to a specific Mental Health Standard ‘People have access to health services that reduce mental health problems and associated impaired functioning.
Key actions
- Coordinate mental health and psychosocial support across sectors.
- Develop programmes based on identified needs and resources.
- Work with community members, including marginalized people, to strengthen community self-help and social support.
- Orient staff and volunteers on how to offer psychological first aid.
- Make basic clinical mental healthcare available at every healthcare facility.
- Make psychological interventions available where possible for people impaired by prolonged distress.
- Protect the rights of people with severe mental health conditions in the community, hospitals and institutions.
- Minimize harm related to alcohol and drugs.
- Take steps to develop a sustainable mental health system during early recovery planning and protracted crises.
Standard 10: Mental health and psychosocial distress (Child protection Minimum Standards 2019)
Children and their caregivers experience improved mental health and psychosocial well-being.
Core Output Indicator 10.2.1: # of individual consultations in UNHCR supported mental health and psychosocial support services
This indicator measures the number of individual consultations in mental health and psychosocial support services provided by UNHCR or its funded partners during the reporting period. The term ‘consultation’ refers to a dedicated and structured contact (a ‘session’) between a person seeking help and a person providing MHPSS services. This includes 1) psychiatric consultations, 2) psychological interventions such as counselling, psychotherapy and brief psychological interventions for individuals, couples and families, 3) community-based activities with the explicit aim to improve mental health and psychosocial wellbeing. It excludes generic activities such as the count of people attending child-friendly spaces or community centres.
Annexes
Learning and field practices
Accessible to UNHCR staff only
This is an online orientation course to strengthen the competencies of health sector actors working in emergencies to establish, support and scale up Mental Health and Psychosocial Support (MHPSS) in emergencies operations (11 modules, 7 hours total).
Links
Main contacts
For questions, please approach the Senior Mental Health and Psychosocial Support Specialist within the Public Health Section in the Division of Resilience and Solutions:[email protected]
In this section:
Let us know what you think of the new site and help us improve your user experience….
Let us know what you think of the new site and help us improve your user experience….
